By David T. Rubin, MD, Professor of Medicine, University of Chicago Medicine
Here are some improvements in testing for SARS-COV-2 and COVID-19 and how I think they will transform what we are doing:
1. Faster Viral Tests for SARS-CoV-2.
Several companies have adapted existing point-of-care tests that can provide results in minutes.
- Faster tests for SARS-CoV-2 may be less sensitive or specific for detecting the virus but we can figure this out.
- Less sensitive means more false negative results (you actually have the virus, but the result says you don’t).
- Less specific means more false positive results.
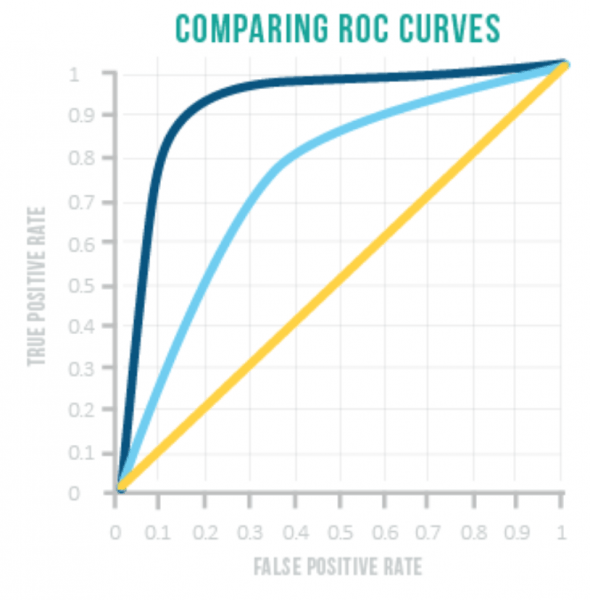
How do you enhance interpretation of a test with less sensitivity and specificity?
You add other information like:
- The clinical scenario (fever, respiratory symptoms, etc.)
- Known exposures (close contact with someone who has COVID-19, being a healthcare worker)
Or you repeat the test after a bit.
To better understand this, think about this in terms of trade-offs:
- In general, the more sensitive a test, the less specific, and vice versa.
- You can read about Receiver Operating Characteristic curves in this helpful article by science writer Karen Steward.1
2. Serologic Antibody Testing.
What is that? Blood tests for your body’s antibodies against SARS-CoV-2!
We know a lot about the immunology of our antibody responses to infections, so here is a slimmed down version:
- When your body is exposed to a foreign antigen, your immune system reacts to protect you.
- The immune system is complex and has both innate (built-in) and adaptive (acquired) defense mechanisms. The adaptive immune system has acute (immediate) and chronic (long-term) responses.
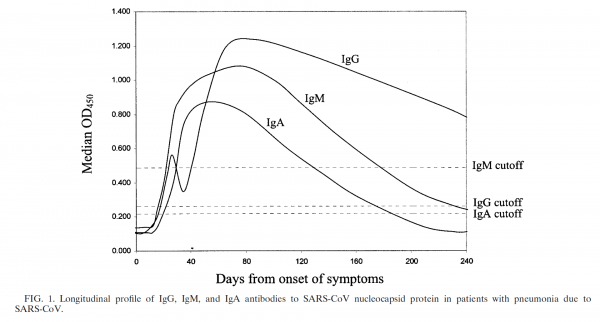
- The acute response of your immune system is the development of antibodies in a class called Immunoglobulin M antibodies (there are others).
- The chronic response is most often characterized by Immunoglobulin G antibodies.
So IgM titers go up first, followed by IgG. - So, in order to know if you are already immune to something, you need to check the IgG titer. Example: many of us are required to have our Hepatitis B IgG titers checked periodically to make sure they remain protected against Hepatitis B.
We believe that people who are infected with SARS-CoV-2 develop the traditional pattern of IgMs and IgGs. How can we know that and what does this mean?
- There are studies looking at this very question from the 1st SARS-CoV outbreak in 2002.2
- It means that if you have measurable IgG antibodies to SARS-CoV-2, you are most likely protected against getting sick with COVID-19. You’ve been immunized against SARS-COV-2.
- In order to get this way, you needed to get exposed to the virus and for many people, that also means getting sick, so this is not the best way to do this but its very important for those who get it.
Wouldn’t it be great if we could get people immunized against SARS-COV-2 without exposing them to the virus?
- Yes, this is how vaccines work- using parts of the virus that stimulate the right part of our immune system, we develop IgGs that protect us.
- We don’t have a vaccine against SARS-Cov-2, but we will get one. In the meantime, knowing who has anti-SARSCoV2 antibodies can provide valuable information, but we need to make sure of a few more things: Are these antibodies truly protective against infection? Do they last?
Once we sort this out, we can do a lot:
- We can identify sick patients with COVID-19 from those who have other problems that can look like it.
- We can identify healthcare workers who are immune and hopefully are protected by their own body against COVID-19.
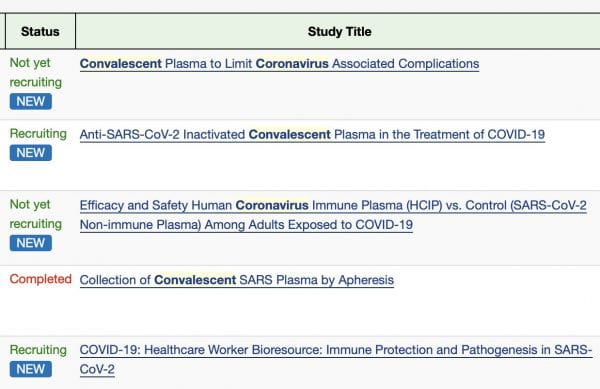
Studies are underway now to use the serum of people who have the anti-SARS-CoV-2 antibodies (IgG) to treat those who are sick with COVID-19 (convalescent serum).3
Thoughts and comments are welcome.
Best wishes,
David
David T. Rubin, MD
Professor of Medicine, University of Chicago Medicine
References:
- Stewart K. Sensitivity vs Specificity. Analysis & Separations from Technology Networks. https://www.technologynetworks.com/analysis/articles/sensitivity-vs-specificity-318222. Accessed March 28, 2020.
- Woo PCY, Lau SKP, Wong BHL, et al. Longitudinal Profile of Immunoglobulin G (IgG), IgM, and IgA Antibodies against the Severe Acute Respiratory Syndrome (SARS) Coronavirus Nucleocapsid Protein in Patients with Pneumonia Due to the SARS Coronavirus. Clin Diagn Lab Immunol. 2004;11(4):665-668. doi:10.1128/CDLI.11.4.665-668.2004
- Search of: convalescent coronavirus – List Results – ClinicalTrials.gov. https://clinicaltrials.gov/ct2/results?cond=convalescent+coronavirus&term=&cntry=&state=&city=&dist=. Accessed March 28, 2020.